Home Resources Culture Change Resources Resources
The resources
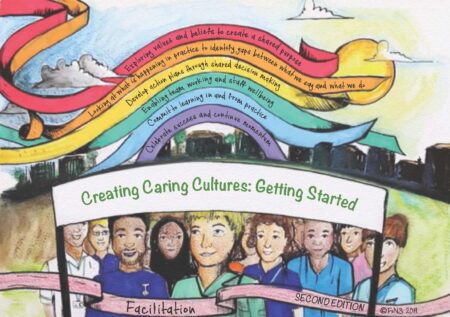
 The resources are based around a model in the form of a rainbow. The model has been developed by FoNS, using our knowledge and experiences over a number of years of working with health and social care teams, helping them to develop workplace cultures that are safe, effective and person-centred.
The resources are based around a model in the form of a rainbow. The model has been developed by FoNS, using our knowledge and experiences over a number of years of working with health and social care teams, helping them to develop workplace cultures that are safe, effective and person-centred.
Each section below contains questions to consider, along with resources and references.
What is culture?
Put simply, culture is ‘how things are done around here’ (Drennan, 1992, p9) – the patterns, habits and routines of practice. Each one of us makes up the culture and so whatever our role, it’s important for everyone to know that as individuals our ideas and actions can change things.
Why do we need to change culture?
One of the most significant factors that influence the quality of care is workplace culture (Manley et al., 2011). This has been highlighted by reports into significant failures in health and social care, which have identified the need for change (Francis, 2013, 2010; Parliamentary and Health Service Ombudsman, 2011; Patterson, 2011).
Although it is often organisational culture that is spoken about, organisations are made up of many smaller cultures, for example within departments and teams and at ward and unit levels (workplaces). It is these cultures that have the greatest influence on the experience of patients, families and staff (Manley et al., 2011).
A caring culture makes things better for everyone. Patients, service users, residents and their families and carers experience good care. Staff feel valued and supported which helps them to provide the care patients want with compassion and confidence.
How do you know if your culture needs to be improved?
The complex nature of health and social care means that wherever you are working, there will always be aspects of care that can be improved, even if there are not any specific concerns. As patients’ needs change, services reconfigure, new staff join the team etc., it is really helpful to continuously reflect on practice to ensure that the care being delivered is safe, effective and person-centred.
Here are some questions that may help you to begin to think about your workplace culture:
- What do patients and relatives say about their experiences of care?
- What do staff say about what it is like to work here?
- What do students say about their experiences of working in your workplace?
- What aspects of care (if any) do you think need to be improved?
- What concerns (if any) do you have about patient safety – falls, pressure ulcers?
- What gaps are there between what people say they do and what actually happens in practice?
- What are the recruitment, retention and sickness rates like?
- How open are staff to change?
You could also look at audits, dashboards, Friends and Family Test, staff surveys, patient surveys, compliments and complaints, exit interviews or use tools such as the 15 Step Challenge (NHS Institute for Innovation and Improvement, 2012) and the ‘Culture of Care’ Barometer (Rafferty et al., 2015).
All of this information will help you to develop a better understanding of your workplace culture, by identifying:
- What is working well and how you could make this happen more often
- What needs to be improved and where you might need support
Wider Resources
Workplace Culture Critical Analysis Tool
References
Drennan, D. (1992) Transforming Company Culture. London: McGraw-Hill.
Francis, R. (2010) Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005 – March 2009. Volume I. London: HMSO.
Francis, R. (2013) Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Executive Summary. London: The Stationery Office.
Manley, K., Sanders, K., Cardiff, S. and Webster, J. (2011) Effective workplace culture: the attributes, enabling factors and consequences of a new concept. International Practice Development Journal. Vol. 1. No. 2. Article 1.
NHS Institute for Innovation and Improvement (2012) 15 Steps Challenge. Retrieved from: http://www.institute.nhs.uk/productives/15stepschallenge/15stepschallenge.html. Last accessed 7th March 2024.
Parliamentary and Health Service Ombudsman (2011) Care and Compassion? Report of the Health Service Ombudsman on ten investigations into NHS care of older people. London: HMSO.
Patterson, M. (2011) From Metrics to Meaning: Culture Change and Quality of Acute Hospital Care for Older People. Report for the National Institute for Health Research Service Delivery and Organisation Programme. London: HMSO.
Rafferty, A., Philippou, J., Fitzpatrick J.M. and Ball, J. (2015) ‘Culture of Care’ Barometer: Report to NHS England on the Development and Validation of an Instrument to Measure ‘Culture of Care’ in NHS Trusts. London: King’s College London.
Getting started with facilitation
Although culture change is not quick and easy, a planned approach helps and it is important that there is someone to guide the process – someone who is enthusiastic, persistent and willing to listen. Maybe this is you.
Because culture is about people, it is important that you work with people, not on your own. If you work alone, you are more likely to take a directive role and to work in a task-focused way, often ending up doing things for staff. However, by adopting an approach that involves using more coaching or facilitation skills, your focus will be on helping staff to become more involved and to take responsibility for improving practice. This may feel harder and more time consuming at first, but we know that skilled facilitation and transformational leadership help to create more effective workplace cultures (Manley et al., 2011).
It is therefore helpful to think about the people that are affected by the culture and/or can affect the culture. For example, patients, service users, residents, families, carers, staff (nursing, medical, therapy, pharmacy, ancillary etc.) and managers etc. Ideally all of these people should be involved, however you may find it easier to begin by working with a small team of interested staff.
There are also other people that can help you. Perhaps there is a practice development team in your organisation or a learning and development department. Your patient experience lead, quality improvement team or research and development department may also be able to offer advice and support. Alternatively, you could start to work with other ward managers or team leaders or make contact with other care home managers. There are also external organisations such as FoNS, that could offer you advice, help and support.
Resources
Activity 1 – Situational Facilitation Characteristic Sheet
Activity 2 – Situational Facilitation Matrix
Activity 3 – Situational Facilitation Strengths and Cautions
References
Manley, K., Sanders, K., Cardiff, S. and Webster, J. (2011) Effective workplace culture: the attributes, enabling factors and consequences of a new concept. International Practice Development Journal. Vol. 1. No. 2. Article 1.
Why are values and beliefs important?
‘How things are done around here’ (i.e. our behaviour) is influenced by our values, beliefs and attitudes. This is often taken for granted – not challenged or spoken about.
Talking to the people who receive care for (patients, service users, residents, families, carers etc.) and the people that give care (nurses, multi-disciplinary team, ancillary staff, managers etc.) about what they think is important (values) and what they feel should happen (beliefs) is therefore an important first step in the process of culture change – helping everyone to think about what they would like care to look like and to begin to think about how they could transform the way things are done to achieve this (Manley, 2000).
This information – about what matters to people – can be used to create a shared purpose.
What is a shared purpose?
A shared purpose sets the direction; aims; and objectives or goals, helping you and your team to identify what you want to move towards.
Who should be involved?
Ideally, a shared purpose should represent the values and beliefs that are held by the people that you care for and the people that you work with. The more people that can be involved in creating the shared purpose, the stronger it will be by (acknowledging differences but):
- Helping people to see what connects them (the shared ground, the common interest) e.g. everyone agrees that mealtimes are an important part of the day, rather than the differences e.g. patients and staff, different job roles etc.
- Creating a personal connection to the change or transformation that you are trying to achieve
How do you do this?
The starting point is getting to know the values and beliefs that people hold about the aspect of care or work that you want to focus on, for example being caring and compassionate, person-centred care, team work, pain management etc.
First, start with yourself – what is important to you and what do you think should happen – what really matters?
Then, invite others to think about their values and beliefs and share them. Perhaps you could use some time in a scheduled meeting and use picture cards to prompt discussion; or maybe you have team days or could allocate some time during education or training. Alternatively you could put up some posters in the office and encourage people to contribute.
Once the values and beliefs have been collected, they can be used to create a shared purpose – providing a focus and energy for any changes or transformations in practice. This is done by finding common values and beliefs, turning these into statements and using these statements to create a shared purpose or vision. At every stage, information should be shared and feedback encouraged.
Below are a number of resources that you could use to help you to work with staff and patients to explore their values and beliefs, and to use these to create a shared purpose.
Resources
Creative approaches to explore values and beliefs
References
Manley, K. (2000) Organisational culture and consultant nurse outcomes: Part 1: organisational culture. Nursing Standard. Vol. 14. No. 36. pp 34-38.
Looking at what is happening in practice and identifying gaps between what we say and what we do
How do I use the shared purpose?
A shared purpose can be used to reflect on or evaluate your current practice – helping you to look at what is happening in practice to identify gaps between what you and your team say and what you do. In effective workplace cultures, the values and beliefs that people hold and talk about are reflected in their behaviour and put into action every day (Manley et al., 2011). That is, what people say is what they do. For example, if a nursing team agree that it is important to know ‘patients as people’:
- You should see staff spending time with patients – asking them about what matters and what is important
- You should hear staff talking about patients as people, not bed numbers or diseases
- Documentation should reflect patient preferences and involvement in decision making
A shared purpose provides a baseline for you to evaluate your current practices and cultures against, helping you to think about and identify:
- What you are doing well and could build upon
- What you might need to create, develop, change or improve to achieve your purpose
How do I do this?
Describing and measuring where you are starting from helps you to identify what you need to change or develop:
- In yourself
- In your team
- In your workplace setting
In most organisations, there is already a lot of activity to ‘measure’ aspects of care and practice, often using audit tools. Whilst this information is useful, it tends to focus on ‘what’ has or hasn’t been done/happened rather than the ‘why’ or ‘how’. For example, a safety cross for pressure ulcers or falls, identifies how many people have acquired a pressure ulcer or fallen, but it does not highlight what is being done well to prevent pressure ulcers, or the circumstances under which people are falling – missing an opportunity to learn in a way that can inform future practice.
Additionally, this activity is often done by only a few people, for example senior members of the team or staff from other departments, who take the data away and interpret it for the team, perhaps making the activity and information that it provides less meaningful to those that it primarily relates to.
To enable culture change it is essential to involve all staff in evaluating practice against your shared purpose. You can do this by looking at what is happening and how things are done (e.g. by observing practice – thinking about what you see, you hear, you feel); by listening to the experience of patients and staff (e.g. asking what has been done well and what could be improved, collecting stories using emotional touchpoints (Dewar et al., 2009)); and by discussing what you find, helping staff:
- To gain new insights
- To deepen understanding
- To identify actions
Resources
Collecting stories using emotional touchpoints
References
Dewar, B., Mackay, R., Smith, S., et al (2009) Use of emotional touchpoints as a method of tapping into the experience of receiving compassionate care in a hospital setting. Journal of Research in Nursing. Vol. 15. No. 1. pp 29-41.
Manley, K., Sanders, K., Cardiff, S. and Webster, J. (2011) Effective workplace culture: the attributes, enabling factors and consequences of a new concept. International Practice Development Journal. Vol. 1. No. 2. Article 1.
Developing action plans through shared decision making
Shared decision-making allows frontline staff to be involved in making decisions about their practice (Swihart, 2011). It acknowledges that they are experts in their area and therefore in the best position to identify solutions to clinical problems and to implement meaningful changes for patients.
Information that is collected about practice should be shared with staff as soon as possible (audits, compliments, complaints, observations, stories etc.), helping them to think about:
- How does current practice relate to the shared purpose?
- What is good/working well and how this could happen more often?
- What are the areas for improvement and ideas for taking action?
Using approaches such as a SWOT analysis (to identify strengths, weaknesses, opportunities and threats) or Claims, Concerns and Issues (Guba and Lincoln, 1989) (to identify positives, concerns and questions) can further inform the planning process by identifying potential barriers but also people and resources that may be able to help and support you. It can also help you to think about how your plans relate to the strategic objectives of your organisation to encourage support and recognition from your senior team.
Action planning is a process that will then help you to identify clear objectives and the steps that will need to be taken to achieve them, considering who should be involved, the resources you will need and the timescale that you should be working towards. When creating action plans, a useful approach is to ask yourself if your objectives are SMART. In other words, are they:
- Specific
- Measureable
- Achievable and Action-orientated
- Relevant and Realistic
- Time-based
Resources
Claims, concerns and issues exercise
SWOT Analysis (strengths, weaknesses, opportunities and threats)
References
Guba, E.G. and Lincoln, Y.S. (1989) Fourth Generation Evaluation. Newbury Park: Sage Publications.
Swihart, D. (2011) Shared Governance: A Practical Approach to Transform Professional Nursing Practice. 2nd Edition. Marblehead, USA: HCPro Inc.
Enabling team working and staff wellbeing
There are strong links between staff engagement (i.e. staff feeling connected with each other and the organisation) and patient outcomes, and staff wellbeing and motivation and patient experience (King’s Fund, 2014; Dixon-Woods et al., 2013; Maben et al., 2012a, b; West and Dawson, 2012). Furthermore, leadership and staff relationships were vital to the ward culture (Maben et al., 2012b).
‘If leaders and managers want staff to treat patients with respect, care and compassion, all leaders and staff must treat their colleagues with respect, care and compassion’ (King’s Fund, 2014, p 10).
It is therefore important to prioritise staff engagement and wellbeing if you want to create a caring culture. Increased staff engagement can be achieved through well structured teams – these are teams that have ‘clear shared objectives, work inter-dependently and meet regularly to discuss effectiveness’ (West and Dawson, 2012). Supportive line management is crucial to the leadership of such teams (West and Dawson, 2012).
Leaders can create positive and supportive environments. This can be enabled by:
- Acting on staff feedback – helping them to act on ideas for making improvements
- Supporting staff development through well-structured appraisals, mentorship, clinical supervision and ongoing learning and education opportunities
- Developing well-defined teams that:
- Have shared goals
- Are clear about their roles and responsibilities
- Creating space for staff to:
- Get to know each other as people
- Reflect on goals, effectiveness, team working, patient care challenges and innovations
A great place to start is by talking to staff – asking them ‘what is it like to work here, what’s good, what could be different?’ Don’t assume that you already know – ask them and really listen. When staff feel listened to and valued, they feel happier at work and we know that if staff are happy then patients are happier too.
You could use existing opportunities to get staff together – team meetings, handovers, huddles during the shift. Or could you be courageous and create new ones – extended coffee breaks, away days, conversation circles? Just do it!
Resources
Thinking about staff wellbeing: enabling team participation
References
Dixon-Woods, M., Baker, R., Charles, K. et al. (2013) Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf. Published Online First doi:10.1136/bmjqs-2013-001947. Retrieved from: http://qualitysafety.bmj.com/content/early/2013/08/28/bmjqs-2013-001947.full. Last accessed on 9th January 2015.
Committing to learning in and from practice
Culture change requires a change in the way things are done – transformations in people and their practice. Learning is crucial to this transformation and the development of caring cultures because it helps us to develop a deeper understanding about ourselves and our practice and we can use this to plan actions (Dewing, 2010).
There are a variety of opportunities to access training and education within health and social care; however many of these are pre-planned by others and often focus on the development of knowledge and skills. It is also not unusual for them to take place away from the workplace.
Whilst these opportunities are essential for the development of competencies, the nature of these approaches may mean that the learning tends to be more general and not specific to the context within which staff are working. This can make it more difficult for staff to translate what they have learnt into their everyday practice – thereby reducing the impact on culture change.
What is not so often recognised is that the clinical area itself makes a great classroom because learning can be facilitated using opportunities arising from everyday practice. This can make the learning more specific to individuals and teams, and to the context within which they are working – perhaps helping people to connect emotionally with the learning, to become more fully engaged and take responsibility for identifying their own actions.
There may already be formal systems in place to facilitate learning in and from practice, for example clinical supervision, preceptorship and mentoring. These can be strengthened and built upon in a number of ways – you can use the shared purpose as a focus. For example by:
- Involving staff in the collection and analysis of audit data
- Involving staff in observing practice e.g. observing mealtimes or the way people speak about each other. It might be helpful to ask people to use their senses e.g. What do you see, hear, smell, feel etc.?
- Asking staff to listen to patient’s experiences of care using:
- Short questions e.g. What did we do well? What would you like us to do more of?
- Emotional touchpoints (Dewar et al., 2009) (see Looking at practice section)
- Encouraging staff to use reflective models
Resources
Using the workplace as a classroom
Learning through critical reflection
References
Dewar, B., Mackay, R., Smith, S., et al (2009) Use of emotional touchpoints as a method of tapping into the experience of receiving compassionate care in a hospital setting. Journal of Research in Nursing. Vol. 15. No. 1. pp 29-41.
Dewing, J. (2010) Moments of movement: active learning and practice development. Nurse Education in Practice. Vol. 10. pp 22-26.
Why should you celebrate success?
Celebrating success is one of the simplest ways to keep teams engaged and motivated. Staff who feel appreciated are more likely to remain engaged and work effectively. We have all heard the expression ‘success breeds success’; teams that focus on and celebrate success create more success – it becomes part of the culture – the way things are done. Staff want to work in successful teams and celebrating reminds them of this.
Celebrating success is also a good way of remembering a shared purpose, helping teams to unify around agreed objectives/goals. It can reinvigorate energy levels and help to maintain momentum.
Leaders have a key role to play in celebrating success. They can facilitate staff engagement and wellbeing by having conversations that focus on the positives, the strengths and the accomplishments of staff. By role modelling praise and recognition in effective and meaningful ways, they can also encourage peers to acknowledge each other too. Staff often know each other well because they work closely together; they are therefore in a great position to recognise when someone has done something well. Peer-to-peer praise can create a thriving and innovative workplace.
What should you celebrate?
There are many things that you can celebrate, but what is most important is getting started. If you wait to celebrate something that you think is really significant, it may be a long time coming and opportunities and momentum could be lost.
You could start by recognising people. Think about what is important to you and start to notice it. Giving feedback that is well prepared, motivating and developmental is a very effective way of celebrating success. This kind of recognition must feel genuine to the person receiving it, and so it should explain exactly what people have done well and be sincere e.g. ‘I saw you communicating very effectively with Mr Brown during his discharge planning. You listened actively and showed kindness and compassion’. You could do this face-to-face or by writing a thank you card or by sending an email. Compliments from patients should always be noticed and shared with individual staff and at handovers or at team meetings. If staff are named personally, copies of thank you cards can be created for their personal files.
You could work with your team to identify small targets – these could be related to your action plans. When these are reached, small celebrations could be planned. For example, creating a poster for display in the staff room, which identifies the people who have been involved, and what they have achieved; you could celebrate with cake or a fruit basket; you could invite your communications department to write a short article about what has been achieved for inclusion in newsletters. Involve the staff in identifying how they would like to celebrate – they may come up with some new and interesting ideas!
Resources
Celebrating success – noticing, appreciating and giving feedback
Find out about FoNS’s programmes for organisations based on the Creating Caring Cultures model