Home News & Views Troubled by nurse retention or lost your joy in nursing or midwifery?
Troubled by nurse retention or lost your joy in nursing or midwifery?
 Claire Johnston, Advisory Board Member Resilience-based Clinical Supervision Programme
Claire Johnston, Advisory Board Member Resilience-based Clinical Supervision Programme
Read our story of how Resilience-based Clinical Supervision can restore and revive every practitioner’s self-esteem
Why do nursing and midwifery leaders hesitate to commit to investment at scale in clinical supervision? Doing it properly may require time, but demoralised nurses will be less productive and more likely to quit. And the bill for ignoring the emotional and psychological safety of NHS staff is eye-watering – turnover alone is costed at £231million a year, to which we can add sickness absence and dysfunctional team working.
So, post-pandemic with nurse retention your number one problem, why wouldn’t you take up a model of restorative supervision which increases self-esteem and critical thinking? Which gives teams the capability to adopt compassionate approaches to caring for one another – and their patients.
If you still need convincing, it is worth remembering that the Nursing and Midwifery Council’s new Future Nurse, Future Midwife and Post-registration Community Nursing specialist standards are built on the regulator’s premise that our universities will be preparing reflective practitioners and that our preceptorship programmes will ‘provide the basis for the beginning of a lifelong journey of reflection’.
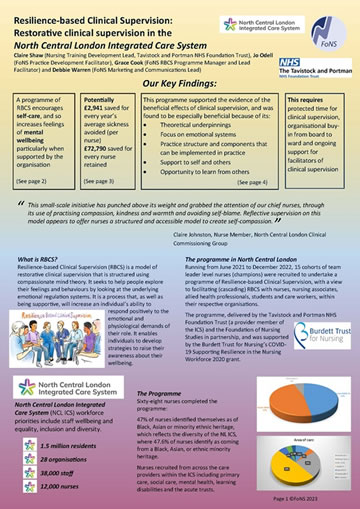
To explore how we might build a model of resilience-based clinical supervision (RBCS) across a single integrated care system, a happy and novel collaboration of North Central London’s Integrated Care Board chief nurse, trust chief nurses, the Foundation of Nursing Studies and a talented nurse therapist from the Tavistock and Portman NHS Foundation Trust made a successful bid for funding to the Burdett Trust.
The aim was to test whether a model of ‘under the surface’ restorative supervision, open to all band 6s and above across our 10 trusts, as well as primary and social care, could offer a non-persecutory, kindly cultural milieu which group members could use to explore their own self-care – and self-neglect.
Equipped with heightened understanding, the group would operate back in their workplaces as facilitators of RBCS, recognising the need for self-compassion, and knowing that we are not only care-givers (where patients are identified as holding all the need) but that we also have needs (conscious and unconscious) in relation to the emotional labour of the work we do.
We had 100 places on offer and 68 nurses completed the programme over 17 months. Given that this was a programme running during the pandemic, we considered this number healthy. Nurses from all environments – acute, mental health, primary and social care – engaged and the split between white and BAME nurses was exactly even. This is something of which we are especially proud.
The theoretical underpinning of the programme was Gilbert’s model of compassion-focused therapy. Anyone interested in learning more will find the Tavistock and Portman’s website a useful source. RBCS is entirely complementary to the professional nursing advocacy approach and we prepare facilitators of RBCS who have trained as PNAs.
An evaluation of the enablers and challenges encountered is now underway, drawing on nurses’ experiences of the programme. Meanwhile a community of practice to sustain the model in practice is now running for the enthusiastic graduates of the programme to come together every month.
 How might you get started on RBCS?
How might you get started on RBCS?
A first step is often just taking the time to notice how you are and to ask others, meaningfully: ‘How are you?’ Instead of ignoring the kind of response which is an everyday experience of a stressed nurse – ‘I’m fine but… I’ve got to get this report done and I haven’t hit the deadline because my time management is so useless, but I will stay on late tonight to finish it’ – the reflective practitioner would truly notice the colleague’s stress and act upon it.
Working together, the two of them would consider possible solutions to this immediate challenge – perhaps delegating some of the report to others, or even questioning whether it is really needed? The stressed nurse will be helped to feel less persecuted, self-critical and self-punishing. Almost all the nurses who went through the RBCS programme afterwards felt confident to run reflective groups for their team or for other multi-disciplinary groups. This small-scale initiative has punched above its weight and grabbed the attention of our chief nurses, through its use of practising compassion, kindness and warmth and avoiding self-blame. Reflective supervision on this model appears to offer nurses a structured and accessible model to create self-compassion.
Visit the RBCS pages to read the review of this North London ICS RBCS project.
Claire Johnston, Advisory Board Member Resilience-based Clinical Supervision Programme – a partnership of the Foundation of Nursing Studies, North Central London ICB & The Tavistock and Portman NHS Foundation Trust.
Comments are closed.

