Home News & Views Promoting staff wellbeing …
Promoting staff wellbeing …
Theresa Shaw, FoNS CEO

On Monday, the Burdett Trust for Nursing held an interesting symposium Strengthening Nurse Leadership & Retention – sadly I couldn’t attend but did follow some of the proceeding on Twitter. The focus was leadership and retention and an important area that I noticed receiving a lot of attention the ability and desire staff may or may not have to continue working – ‘being fit to work’. not just physically but having the emotional capacity to work – feeling resilient.
I was pleased to see that Gemma Stacey presented the work she led with colleagues to implement a model of Resilience Based Clinical Supervision (RBCS). This is a form of clinical supervision which focuses on the ‘emotional systems motivating the response to a situation’ and includes elements of mindfulness-based exercises with a view to ‘enhancing well-being, resilience and improving patient care’. FoNS is very pleased to host the range of resources for those interested in using the approach and I certainly recommend you take a look (see the link above).
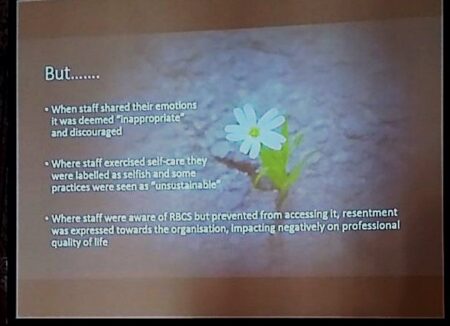 However, sharing the details about RBCS is not the real focus of my blog rather I wanted to come back to the issues relating to wellbeing, self-care and resilience. One of Gemma’s’ slides posted on Twitter (right) gave insight to some interesting findings. While there are many positive benefits for those who experience RBCS, it also revealed what could be described as negative consequences: Where staff exercised self-care, they were labelled selfish and some practices were seen as ‘unsustainable’. Reading this prompted me to think about the extent to which staff wellbeing and the adoption of ways of working that encourage staff to take care of themselves and feel a sense of resilience is really being attended to across our health and social care services?
However, sharing the details about RBCS is not the real focus of my blog rather I wanted to come back to the issues relating to wellbeing, self-care and resilience. One of Gemma’s’ slides posted on Twitter (right) gave insight to some interesting findings. While there are many positive benefits for those who experience RBCS, it also revealed what could be described as negative consequences: Where staff exercised self-care, they were labelled selfish and some practices were seen as ‘unsustainable’. Reading this prompted me to think about the extent to which staff wellbeing and the adoption of ways of working that encourage staff to take care of themselves and feel a sense of resilience is really being attended to across our health and social care services?
When I’m talking about ways we can improve care and services, I find myself constantly referring to the importance of supporting staff and seeking ways to help them give of their best. Indeed, there is a remarkable volume of literature, research, evidence, narrative in relation to the wellbeing of staff and quality of care and services – if in doubt just type ‘staff wellbeing and care quality’ into a search engine and cast your eyes over the vast array of material.
As far back as 2013, the National Nursing Research Unit (Kings College London) published study report ‘Does NHS staff wellbeing affect patient experience of care?’. This work strongly suggested that there is a relationship between staff wellbeing, their ability to deliver care and the quality of the patient experience.
More recently, many researchers include Jill Maben and Michael West, along with a number of respected organisations including the King’s Fund, the Health Foundation, the Picker Institute, the Royal College of Physicians and the Point of Care Foundation, have highlighted clear evidence that the wellbeing, satisfaction and experience of staff directly impacts on their ability to offer high quality, safe and effective care. Arguably the case is overwhelming!
However, we also know that the translation of evidence into practice is not easy; simply reading evidence or hearing about potential ways of changing practice rarely changes things. In order to change, we, as people, need to feel/be in a relatively good place – valued, supported, happy and safe, all these help us feel more open and receptive to challenge and change. Intervention like RBCS can help and if organisations support its use, they are doing their bit to help staff give of their best.
But, I also believe there are more fundamental ways in which we need to challenge our thinking. As I was looking at the evidence on staff well-being I also came across a thought-provoking editorial posted by the Nursing Times Student Editor Adam Roxby in 2011 entitled: ‘Should we all be a little more selfish?‘ Adam described what he saw in the NHS at the time as ‘healthcare martyrdom … this pervasive culture which has permeated our hospitals makes nurses sacrifice their sanity on a regular basis’. He witnessed staff missing breaks, working late and so on and asked himself ‘So who is my priority? Is it my patients? My family? Or should it be me?’
I think, and I have said in a few arenas, that I often wonder if there was point around the late nineties early noughties when staff were not seen as a priority and so stopped prioritising themselves? Phrases like ‘putting the patient at the centre’, ‘the needs of the patients are the priority’ and ‘you are here for the patients first and foremost’ are hard to disagree with, but what messages did/do they send to staff – you are here to deliver a service and your needs don’t matter?
I do think there are areas where we are making progress but there is still much more we need to do and part of this is being honest about what is happening to staff in practice. Everyone has a role because the truth is everyone is affected by the demands that working in health and social care put on everyone in an organisation, no matter what their role. The idea that connecting emotionally should be discouraged or that self-care might be selfish saddens me because it is this emotional connection and awareness that gets to the heart of caring and the high quality services I believe staff working across health and social care have at their core.
Comments are closed.