Home News & Views Enhancing staff wellbeing: What works?
Enhancing staff wellbeing: What works?
Kate Sanders and Jo Odell, Practice Development Facilitators, FoNS

Kate Sanders

Jo Odell
In November 2018, the Foundation of Nursing Studies, in collaboration with the Point of Care Foundation, hosted a tweet chat with a focus on “what enhances staff wellbeing”. This is a topic that both organisations place great emphasis on when working with staff across all aspects of health and social care. Following the chat some initial impressions were published. Both organisations then individually undertook a more in-depth analysis of the comments and conversations that followed. Here are the key themes that emerged from the FoNS analysis.
Staff wellbeing is enabled by:
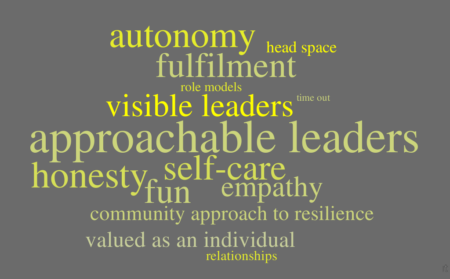
- Individuals feeling valued as an individual but also feeing part of a team; having a sense of autonomy, fulfilment and meaning in their work; having fun and experiencing joy at work; being able to self-care
- Leaders who are visible and approachable and who act with empathy and compassion; act as role models by being brave, open and honest; are effective communicators, listening and engaging with staff view points; and who are reflective and constructive
- Workplace and organisational cultures that value investment in staff wellbeing, recognising the return on this investment. This includes recognising the importance of relationships, and control and autonomy over work
- A system or community approach to the development of resilience
- ‘Time out’ and ‘head space’ away from practice, both formal and informal, to listen, to learn, to reflect, to be
Several of these themes resonate with three core human needs to enhance staff experience in the workplace, identified by Dr Michael West in his recent blog in response to the publication of the latest NHS staff survey data. These needs are ‘belonging, competence and autonomy’. Dr West argues that when: ‘these needs are met in the workplace, people are more intrinsically motivated and have better health and wellbeing.’
Recent years have seen an increasing amount of evidence relating to the importance of staff wellbeing and its relationship with patient outcomes and experiences. For example, a new publication by the NHS Staff and Learners’ Mental Wellbeing Commission (NHS Health Education England, February 2019, p 2), which reports on research with staff and family members of those employed by the NHS, is underpinned by an extensive review of the literature on mental wellbeing at work. As with other reports (King’s Fund (2014), this report highlights that ‘that happy staff are more compassionate and provide safer care’. Several of the key themes (see pp 10-11) also back up the findings from our tweet chat. And yet, like others, our experience of working with nurse-led teams in health and social care is that there is an increasing gap between the evidence of what should happen and what is experienced by staff in relation to whether their wellbeing is prioritised by their services and organisations.
So how can individuals and teams, take a collective approach to leadership and create their own opportunities however small, to facilitate wellbeing?
The NHS Staff and Learners’ Mental Wellbeing Commission highlight that ‘the simple things’ are important. As highlighted by the tweet chat, making time for people is important and valued. What simple things can we do to achieve this?
- Taking time to ask people how they are and really listening to their response?
- Saying thank you, being specific about what you are thankful for?
- Noticing and acknowledging when people need extra support and taking time to respond?
Thinking more about the need for ‘belonging, competence and autonomy’, we have come up with some ideas that might be helpful:
- Prioritise time to discuss difficult situations as a team – to learn and to support
- Develop buddying systems to enable every member of the team to have regular 1:1 time, to talk about how they are feeling about their role and their work – this could be with a leader or a peer
- Create regular opportunities for reflection, individually or in a group, using clinical supervision
- Explore your values and beliefs as a team
- Plan regular team meetings that enable staff discussion, reflection on practice and shared decision-making
We welcome your suggestions and are here to provide support in terms of resources and talking through how you might get started:
References
Michael West blog: The NHS crisis of caring for staff: what do we need to do? London: The King’s Fund. https://www.kingsfund.org.uk/blog/2019/03/nhs-crisis-caring
King’s Fund (2014) Developing Collective Leadership for Health Care. London: King’s Fund. p 10. Retrieved from: https://www.kingsfund.org.uk/publications/developingcollective-leadership-health-care. Last accessed 24th January 2019.
Comments are closed.

